Healthcare organizations face a complex web of payer agreements that present significant legal and regulatory risks. From Stark Law compliance to Anti-Kickback requirements, these contracts require careful monitoring to avoid penalties and operational disruptions.
Experian Health cites bad data as the primary issue that leads to denials.
Top 3 reasons for denials:
46%
Missing or inaccurate data
36%
Authorizations
30%
Inaccurate patient info
Despite these critical implications, many organizations manage agreements through scattered spreadsheets and email threads, creating substantial vulnerabilities. While resources pour into clinical outcomes, the contracts that fund that care are often overlooked. The result? Missed renewals, undetected underpayments, and shifting authorization rules that catch providers off guard.
This guide will walk you through how effective payer contract management can help you turn agreements into strategic tools for growth, protecting revenue, improving visibility, and giving you the leverage you need at the contract negotiation table.
What is payer contract management?
Payer contract management is the process of creating, tracking, and optimizing agreements between healthcare providers and insurance companies. These contracts outline everything from reimbursement rates and fee schedules to prior authorization rules and regulatory requirements. Managing them well means fewer denials, faster payments, and better margins.
Employment law is complex, and representing physicians complicates it even further because physicians are subject to more stringent regulations than other employees. Your lawyer needs to be someone who does physician employment contracts.
These legally binding agreements establish complex frameworks that govern reimbursement methodologies, regulatory compliance obligations, and mutual legal responsibilities, all of which must align with federal and state healthcare laws and regulations.
The payer contracting process extends beyond the signing of a simple agreement – it requires continuous monitoring, performance analysis, and proactive management to ensure favorable contracts that support your organization’s financial objectives.
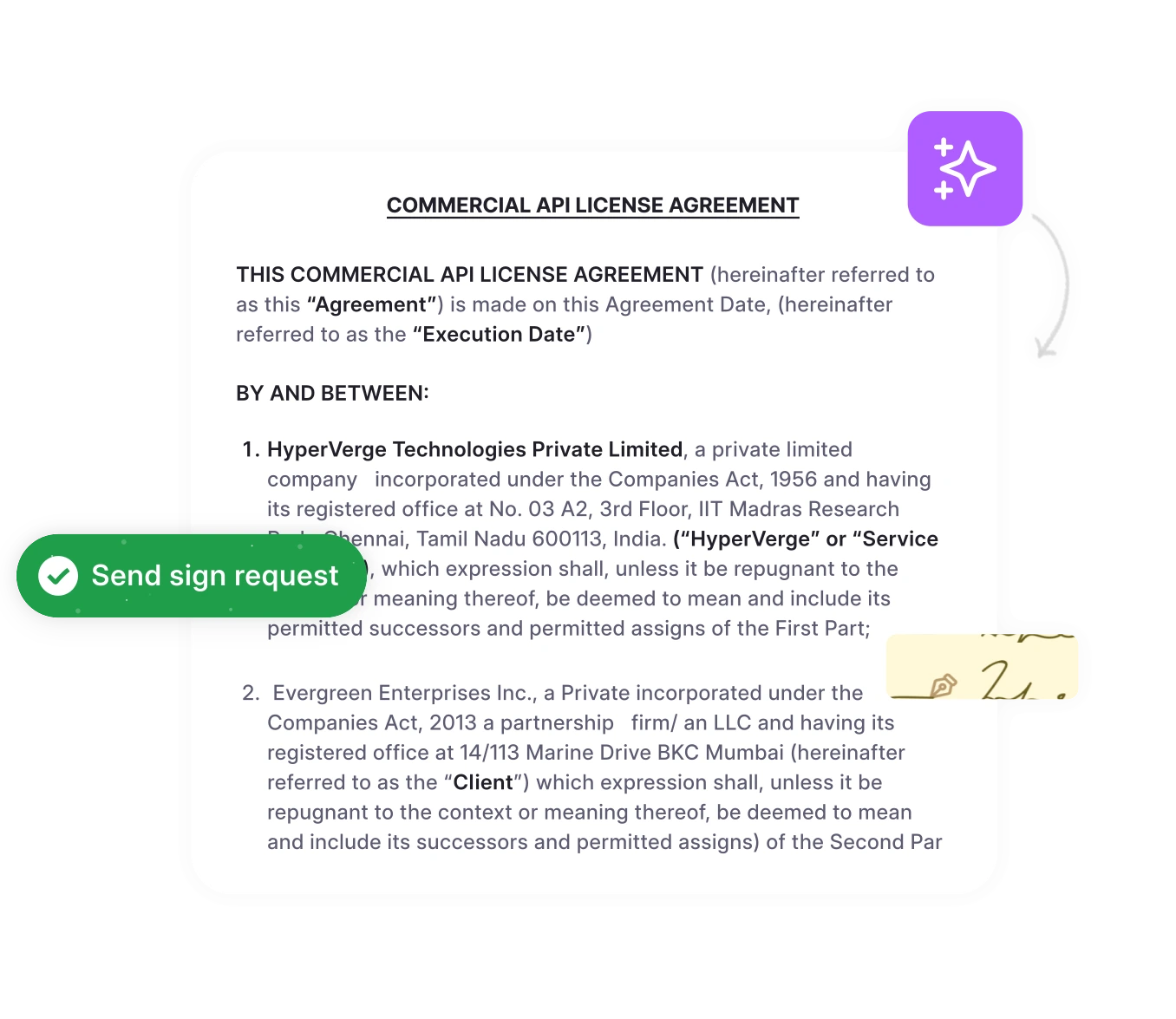
Set automated renewal alerts in advance
With HyperStart, track upcoming expirations, renegotiate rates proactively, and avoid last-minute rush during renewals.
Book a DemoWho are the types of payers in healthcare contract management?
Understanding the diverse landscape of payers is essential for developing effective contracting strategies. Each payer type presents unique challenges and opportunities that require tailored approaches to contract negotiations and ongoing management.
| Payer | Highlights |
| Commercial Insurance (BCBS, Aetna, Cigna) | Private insurers offer comprehensive coverage with varying deductibles, copays, and network restrictions. Contracts include complex reimbursement structures and quality metrics. |
| Medicare | Federal program for adults aged 65 and older and individuals with disabilities. Standardized fee schedules with limited room for negotiation. Includes Medicare Advantage plans with additional contract variations. |
| Medicaid | State-administered program for low-income individuals and families. Reimbursement rates are typically lower than commercial payers with extensive prior authorization requirements. |
| HMOs (Health Maintenance Organizations) | Require patients to select primary care physicians and obtain referrals for specialists. Often, capitated payment models emphasize preventive care coordination. |
| PPOs (Preferred Provider Organizations) | Allow patients to see any provider but offer better coverage for in-network services. Typically use fee-for-service models with negotiated discount rates. |
| Self-funded ERISA Plans | Employer-sponsored plans where companies assume financial risk. Often managed by third-party administrators with customized contract terms and payment structures. |
How to optimize payer contract management in 7 steps
Here’s how you can transform your approach to payer contract management from reactive to proactive, aligning it with a contract lifecycle management process that is systematic and measurable.
Step 1: Centralize and organize all payer contracts
Successful contract management begins with centralization. Import existing payer agreements from email, drive, or practice management systems. Use AI-powered automation to extract key metadata like reimbursement rates, prior authorization requirements, and renewal dates through contract data extraction.
This approach helps organizations create a searchable repository for all commercial, Medicare, and Medicaid contracts, providing the knowledge base needed for effective decision-making.
Step 2: Set up automated payer contract tracking
Good intentions go to die in manual review. You start with the best of intentions—spreadsheets, calendar reminders, sticky notes—but life gets busy, and things fall through the cracks.
Set up alerts for contract renewal deadlines, rate increase opportunities, and amendment notifications. Track payer-specific obligations like quality reporting requirements and performance metrics. The goal is to make compliance and opportunity identification automatic, not accidental.
Step 3: Implement payer performance monitoring
Track key metrics for each payer: average payment times, denial rates, reimbursement accuracy, prior authorization approval rates, and processing times.
When you can see patterns in payer behavior, you can make informed decisions about which relationships to prioritize, which contracts to renegotiate, and which payers might be violating their contract terms.
Step 4: Establish payer contract compliance workflows
Each payer type has specific regulatory requirements; Medicare has its own rules, Medicaid has state-specific requirements, and commercial payers have their own compliance standards.
Create systematic contract approval workflows that ensure you’re meeting all requirements. Build audit trails for all payer interactions and contract modifications. This proactive approach to compliance reduces risk and helps you avoid costly penalties while maintaining access to essential payer networks.
The HHS Office of Inspector General provides comprehensive compliance guidance, emphasizing that effective compliance programs require systematic monitoring of contractual obligations and regulatory requirements.
(Source: U.S. Department of Health and Human Services)
Step 5: Optimize payer collaboration and communication
Your billing team, clinical staff, and administrative personnel all need to understand and work with agreements daily.
Make contract terms easily accessible to relevant stakeholders. Integrate your contract data with your EHR and practice management systems. Streamline communication workflows for contract amendments and rate negotiations. The goal is to make contact information a living, breathing part of your operations.
Step 6: Analyze payer contract performance and profitability
Compare reimbursement rates across different payers for the same services. Identify which payer contracts offer the most favorable contracts and the highest profitability. Track contract value realization and identify revenue recovery opportunities.
This analysis helps you understand which agreements are worth the effort and where you should focus your negotiations.
Step 7: Prepare for payer contract renewals
Use historical performance data to strengthen renegotiation positions with underperforming payers, leveraging these contract negotiation strategies to secure better terms. Set up 90-day advance notifications for contract expirations to allow adequate preparation time for strategic renewal discussions.
Leverage contract analytics to negotiate better rates and terms based on documented performance and market benchmarks. This proactive approach to renewals ensures organizations maximize their negotiating power and secure favorable contract terms.
Before signing any managed care contract, a medical practice should consult with a healthcare lawyer who has relevant experience. Specific provisions in third-party payer contracts can significantly impact a provider’s revenue stream.
Payer contract management challenges and solutions
Let’s be honest about the challenges you’re facing. These are real issues that impact your bottom line and your ability to serve patients effectively.
| Challenge | Solution |
| Manual tracking leads to missed opportunities | Implement automated contract management software with real-time monitoring and intelligent alerts. Ensure critical deadlines are not missed. Watch contract performance and compliance. |
| Complex contract terms create confusion | Deploy AI-powered contract analysis tools to extract key terms, summarize reimbursement information, and highlight compliance requirements in plain language. |
| Underpayments go undetected | Implement automated claims matching and variance detection systems with instant underpayment alerts to identify discrepancies immediately and trigger workflows for revenue recovery. |
| Contract renewals catch providers off guard | Establish proactive contract renewal management with 90-day advance notifications and structured renegotiation reminders to ensure adequate preparation time and negotiation leverage |
| Lack of payer performance visibility | Deploy comprehensive analytics dashboards comparing payer performance across payment times, denial rates, and reimbursement accuracy to enable data-driven decision-making and strategic payer relationship management. |
Go from “We’ll Check” to “We Know”
See, track, and act on underpayments, denials, and payer performance in real-time with HyperStart’s AI-powered dashboards.
Book a DemoEssential features of payer contract management software for legal compliance
The ideal contract management software for healthcare organizations should incorporate these capabilities to ensure compliance, maximize reimbursement, and minimize administrative friction.
1. Payer contract repository
Centralized storage for all payer agreements with advanced search capabilities to quickly find specific reimbursement rates, prior authorization rules, and coverage limitations across multiple insurance plans.
2. Claims-to-contract reconciliation
Automated matching of insurance payments against contract terms to identify underpayments, incorrect reimbursement rates, and payer compliance issues in real-time.
3. Payer performance analytics
Comprehensive dashboards tracking key metrics like average payment time, denial rates, prior authorization approval rates, and reimbursement accuracy by individual payer.
4. Contract renewal management
Proactive tracking of payer contract expiration dates with automated alerts 90+ days in advance, plus workflow management for negotiations and rate increase requests.
5. Fee schedule comparison
Side-by-side analysis of reimbursement rates across different payers for the same CPT codes, helping identify which contracts offer the most favorable terms for specific services.
Best practices for payer contract management
1. Establish proactive contract monitoring
43% providers are extremely concerned about receiving full reimbursements because of frequent changes to pre-authorization rules and other payer policies.
What this looks like in practice:
- Establish Key Performance Indicators (KPIs) for each payer relationship and automate obligation tracking
- Schedule quarterly contract performance reviews for each major payer
- Set up automated alerts for payment variances exceeding 5% of expected amounts
- Create monthly dashboards showing reimbursement trends, denial patterns, and payment timing
2. Maintain centralized contract documentation
If you’ve ever spent 20 minutes hunting for a contract amendment while a payer representative waits on the phone, you understand why centralization matters. But true centralization goes beyond just storing documents in one place.
Your centralized repository should include:
- Original contracts and all amendments
- Historical performance data
- Negotiations notes and contract audit trails
Version control is critical. You need to know which contract terms are in effect and what changes are pending. Consider this scenario: you’re reviewing a denied claim, but you’re looking at last year’s contract language.
3. Implement systematic underpayment tracking
Compare actual payments against contract terms monthly to identify and recover lost revenue quickly.
Build a robust underpayment detection process:
- Compare and report on actual payments against contract terms
- Track appeal success rates and recovery amounts by payer
- Document patterns that might indicate system issues or contract violations
4. Prepare data-driven renewal strategies
Contract renewals are your opportunity to reset the relationship, improve terms, and secure better reimbursement rates. Yet many providers treat renewals as administrative tasks rather than strategic opportunities.
The 90-day renewal preparation process:
Days 90-61 before expiration:
- Gather comprehensive performance data for both your organization and the payer
- Analyze reimbursement rates against market benchmarks
- Document any compliance issues or support problems
- Research the payer’s current market position and priorities
- Identify your negotiating strengths and potential concessions
Days 60-31 before expiration:
- Prepare detailed performance presentations
- Draft improved terms
- Assess your risk tolerance for various scenarios with legal and finance teams
- Schedule preliminary discussions with payer representatives
Days 30-0 before expiration:
- Conduct formal negotiations
- Document all proposed changes
- Review final contract terms with stakeholders
- Plan the implementation of any new requirements
- Communicate and sign off on changes
5. Monitor payer compliance continuously
Contracts create mutual obligations, but payers often get away with not meeting their commitments because providers don’t systematically track and enforce contract compliance. Change this dynamic, and you change your financial performance. Key accountability metrics to track:
- Payment timing: Most contracts specify payment timeframes (typically 30–45 days). Track actual payment times and flag systematic delays. Late payments cost you money through cash flow impacts and administrative burden.
- Denial patterns: Monitor denial rates by procedure, provider, and reason code. Unusual spikes often indicate system issues, policy changes, or training problems that the payer should address.
- Prior authorization performance: Track approval rates, processing times, and appeals success rates. Payers who consistently delay or deny appropriate authorizations are violating the spirit, if not the letter, of your agreements.
- Customer service quality: Document response times to inquiries, knowledge levels of representatives, and resolution rates for claims issues. Poor service impacts your operational efficiency and should be part of renewal discussions.
Modern payer contract management software offers healthcare providers the tools they need to:
Get HyperStart for payer contract management
HyperStart’s AI-powered contract management platform provides all the tools you need to implement these seven steps effectively. From automated contract extraction and tracking to advanced analytics and collaboration features, we help healthcare organizations optimize their payer relationships and maximize revenue.
Key benefits:
- 80% reduction in contract administration time
- Never miss a renewal with automated tracking and alerts
- Real-time analytics for data-driven payer relationship decisions
Book a Demo to see how HyperStart can revolutionize your payer contract management process.